Juvenile

About Juvenile Scoliosis
Juvenile scoliosis is an idiopathic scoliosis that affects children between the ages of 4 and 10. Like other types of scoliosis it is characterised by an abnormal sideways S or C curve of the spine.
Juvenile scoliosis is more often seen in girls than boys. In children between the ages of 4 to 6 years the rate is fairly equal between the two sexes. However between the ages of 6 to 10 years the rate is much higher among girls.
It is seen more frequently than Infantile Idiopathic Scoliosis, but it is less common than Adolescent Idiopathic Scoliosis.
Mild scoliosis does not usually cause significant back pain in children. However some discomfort and stiffness is not uncommon.
Curves tend to bend to the right in children with juvenile scoliosis, however left curves tend to have a better prognosis.
Children with juvenile scoliosis generally have a high risk of progression of their curve. Research has shown that a large number children with this condition will worsen and require active treatment, with juvenile curves almost never resolving spontaneously.
The best chance to correct scoliosis is with early detection and treatment as they grow. This makes regular screening for the signs of scoliosis, early detection and proper management of high importance.
In many cases, treatments such as custom bracing and scoliosis specific exercise rehabilitation are available as evidence-based treatment options for patients with Juvenile Scoliosis.
What Causes Juvenile Scoliosis?
The exact cause of juvenile scoliosis is unknown hence its classification as an “idiopathic” scoliosis. Idiopathic means “of unknown cause”. However, the juvenile form has similar clinical features to adolescent scoliosis and the two conditions actually have a number of the same proposed causes. This has led to juvenile idiopathic scoliosis sometime being referred to as “early onset adolescent idiopathic scoliosis”.
The most widely accepted theory about the development of Juvenile and Adolescent Scoliosis is one involving genetic inheritance. Scientists believe that a set of genes that cause scoliosis may be inherited.
However, scoliosis does not always appear in subsequent generations i.e. not every child of parents who have scoliosis will develop the condition. This suggests that individuals are affected by these genes to different degrees and that other factors may be required for a scoliosis to develop.Research has uncovered several different genes on that appear to be associated with scoliosis and genetic tests that can identify these genes are currently being trialed.
If you’ve noticed a change in a loved one, or have a family history of scoliosis, we’re here to answer any questions you may have. Contact Us.

How is Juvenile Scoliosis Diagnosed?
Juvenile idiopathic scoliosis is usually first suspected by the parents of a child, who may notice uneven shoulders or hips, or one shoulder blade more prominent than the other. Examination by a health professional can also discover a juvenile scoliosis. A common test used to screen for scoliosis is called the “Adams forward bending test”. A scoliosis clinician will include this test as part of their full assessment at an initial consultation. ScoliCare has a free screening app called ScoliScreen that can assist when doing this visual assessment at home.
In this test the child bends forward at the waist until the spine is parallel with the floor, while the examiner observes the shape of the spine as it bends.
- The main feature alerting the examiner to a scoliosis is the presence of a rib hump, which is typically seen in a thoracic scoliosis. A rib hump is where the ribs on one side protrude more compared to the other side when the child is bent forward. In some cases the scoliosis is not in the upper part of the torso but in the lower back. Therefore screening should also consist of examination of the whole upright posture including the level of the hips.
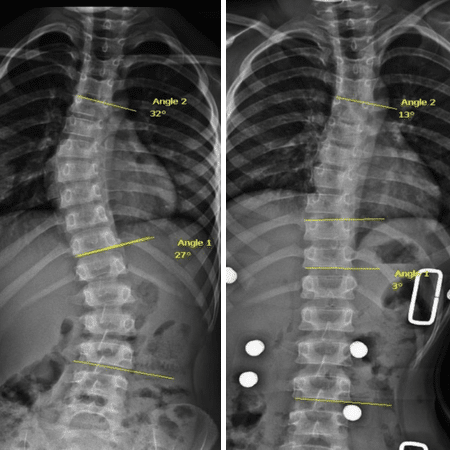
- When scoliosis is suspected, a careful neurological exam should always be carried out, with further investigation as needed, to ensure that the scoliosis is not the result of a neurological condition. X-Rays should also be taken standing up to give a true representation of the curve under the load of gravity. X-rays also give clear images of the bones and allow for more precise measurements of the curvature.

Treatments for Juvenile Scoliosis
ScoliBalance® is a specialised scoliosis specific exercise program that is tailored to each individual patient according to their curve type, symptoms and treatment goals.
In juvenile curves between 10 and 20 degrees, there is evidence to suggest that an intensive course of scoliosis specific exercise rehabiliation may be able to make some correction or control the curve.
However once the curve is greater than 20 degrees it is usually too large for rehabilitation alone to manage, and ScoliBalance in conjunction with bracing treatment may be recommended.

Larger, progressive curves may require full-time wear of a custom 3D designed over-corrective brace to help control the curve, slowing progression and delaying surgery until suitable maturity. A custom over-corrective brace offers an opportunity to work aggressively with large curves and potentially make some correction depending on the flexibility of the curve.
Occasionally with juvenile scoliosis, bracing may be discontinued for one or more years, with a return to observation. As the child begins an adolescent growth spurt, they may be re-braced to maintain the previously achieved correction of the curve as they grow. For curves that continue progressing during bracing treatment, surgery may be in the patient's best interest.
Specific scoliosis exercise rehabilitation, such as ScoliBalance® , may also be used in conjunction with bracing treatment.
In such cases, the most appropriate initial treatment is serial casting, which entails that a cast be applied and changed every 6 to 12 weeks, in an attempt to gradually correct the curvature. The cast is made of plaster and is applied in the operating room under general anaesthesia, which means that the child will be put to sleep through the application process so as to minimise discomfort.
Casting treatment is followed up with bracing treatment which is needed to maintain the correction.

In juvenile cases, special rods called “growing rods” can be used in an attempt to maintain correction and allow growth.
In this type of treatment a metal rod attached to the spine is periodically lengthened by a simple procedure. This correction without fusing the spine minimises the stunting of growth that can occur with spinal fusion.
If the curve is large and the child is of reasonable maturity, a definitive spinal fusion may be recommended. This involves fixing rods to the spine to stop movement and may require a bone graft.


