Adolescent

About Adolescent Idiopathic Scoliosis (AIS)
Adolescent Idiopathic Scoliosis (AIS) is a scoliosis that affects children or adolescents from the age of 10 into young adulthood. Typically it is noticed around 11 to 12 years of age in girls, and a little later in boys.
Like other types of scoliosis, AIS is characterised by an abnormal sideways S or C curve of the spine. Children with AIS are generally otherwise healthy.
AIS is the most common type of scoliosis. Up to 5% of all children between 10 and 18 years old will develop this type of scoliosis*. It is also more commonly seen in girls than boys – 90% of scoliosis cases are girls.
AIS also often begins to develop at the initial onset of puberty, and can progress rapidly during periods of growth.
In children and adolescents, the best chance to correct scoliosis is with early detection and treatment as they grow. This makes regular screening for the signs of scoliosis, early detection and proper management of high importance.
In many cases, treatments such as custom bracing and scoliosis specific exercise rehabilitation are available as evidence-based treatment options for patients with AIS.
*Konieczny MR, Senyurt H, Krauspe R. Epidemiology of adolescent idiopathic scoliosis. Journal of Children’s Orthopaedics. 2013;7(1):3-9.
What Causes Adolescent Idiopathic Scoliosis?
The exact cause of adolescent scoliosis is unknown hence its classification as an “idiopathic” scoliosis. Idiopathic means “of unknown cause”.
The most widely accepted theory explaining the development of adolescent scoliosis is one involving a genetic trigger. Adolescent scoliosis is often seen occurring in members of the same family, in the same and in past generations. Scientists believe that a set of genes that may trigger scoliosis may be inherited.
However, scoliosis does not always appear in subsequent generations i.e. not every child of parents who have scoliosis will develop the condition. This suggests that individuals are affected by these genes to different degrees and that other factors may be required for a scoliosis to develop. Research has uncovered several different genes that appear to be associated with scoliosis and genetic tests that can identify these genes are currently being trialed.
If you’ve noticed a change in a loved one, or have a family history of scoliosis, we’re here to answer any questions you may have. Contact Us.

How is AIS diagnosed?
In the absence of school screenings, adolescent scoliosis is usually first noticed by the child or a family member of the child. A common test used to screen for scoliosis is called the “Adams forward bending test”. A scoliosis clinician will include this test as part of their full assessment at an initial consultation. ScoliCare has a free screening app called ScoliScreen that can assist when doing this visual assessment at home.
In this test the child or adolescent, bends forward at the waist until the spine is parallel with the floor. The examiner stands behind the child and observes the shape of the spine as they are bend over.
- The main feature alerting the examiner to a scoliosis is the presence of a rib hump, which is typically seen in a thoracic scoliosis. A rib hump is where the ribs on one side protrude more compared to the other side when the child is bent forward. In some cases the scoliosis is not in the upper part of the torso but in the lower back. Therefore screening should also consist of examination of the whole upright posture including the level of the hips.
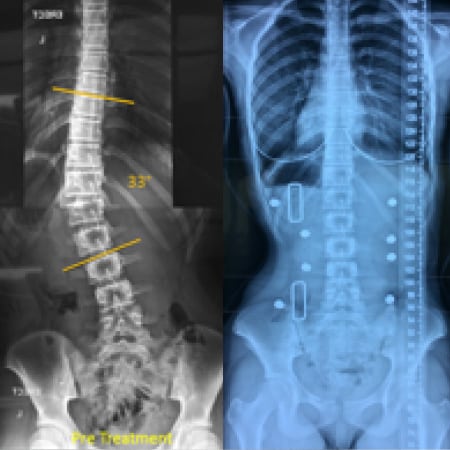
- When scoliosis is suspected, a careful neurological exam should always be carried out, with further investigation as needed, to ensure that the scoliosis is not the result of a neurological condition. X-Rays should also be taken standing up to give a true representation of the curve under the load of gravity. X-rays also give clear images of the bones and allow for more precise measurements of the curvature.

Treatments for Adolescent Idiopathic Scoliosis
Scoliosis clinicians can assess this process by examining the hand and/or pelvis bones on X-rays. They use these X-rays to determine what is known as the Risser sign, which helps grade the level of maturity of the skeleton.
As a general rule, the more immature the skeleton, the more growth left and the greater potential for progression. If a large curve (e.g. 40 degrees) is present in an immature Risser 0 patient it would have a very high likelihood of progression and require intervention, compared to the same 40 degree curve which could be present in a skeletally mature Risser 5 adolescent that did not require intervention, because the chance of progression is extremely low.

ScoliBalance® is a specialised scoliosis specific exercise program that is tailored to each individual patient according to their curve type, symptoms and treatment goals.
In the case of small adolescent idiopathic curves of less than 20 degrees, ScoliBalance may help to stop the curve from progressing and improve posture and body cosmetics
In larger curves, generally greater than 20 degrees, ScoliBalance can be used in conjunction with bracing. The program complements brace wear, and helps maintain the correction achieved with bracing, as well as improving muscle endurance and spinal flexibility.

In some cases, small curves in younger children may be managed by a custom 3D designed scoliosis brace, worn only at night. This would be limited as an early intervention for smaller curves in younger patients.
Larger, progressive curves may require full-time wear of a custom 3D designed over-corrective brace to help manage or reduce the curve and/or reduce the chances of surgery.
Specific scoliosis exercise rehabilitation, such as ScoliBalance®, may also be used in conjunction with bracing treatment. The program complements brace wear, and helps maintain the correction achieved with bracing, as well as helping to improve muscle endurance and spinal flexibility.
In adolescent curves greater than 45 degrees conservative treatment becomes more difficult. At this point the type of treatment can vary depending on the treatment goal. For example if the patient is Risser 0 with a 50 degree thoracic curve they are entering the surgical zone, but being immature it may be desirable to delay surgery until Risser 3/4. Therefore a custom brace and specific exercise rehabilitation may be recommended to try and reduce and stabilise the curve until the patient is more mature and ready for surgery. In a more mature patient Risser 4 with the same 50 degree curve the surgeon may feel that the spine is well balanced and if the curve can be maintained at its current position that surgery may not be necessary.
Generally in large curves with significant growth left, the prognosis for conservative treatment is usually poor and the primary treatment goal becomes to control the curve and slow progression, delaying surgery until suitable maturity.