56 year old female patient with de novo degenerative scoliosis.
Postural improvement, improved mobility and reduced pain in a female patient with de novo degenerative scoliosis using a 3D designed custom brace
Summary:
This case demonstrates the successful management of a patient with de novo degenerative scoliosis. The patient presented with a long history of back and leg pain which were interfering with her activities of daily living. The patient had a 51° (Cobb) left lumbar scoliosis with laterolisthesis and marked degenerative change throughout the lumbar spine. There were alterations to the normal lordosis and kyphosis angles, as well as coronal and sagittal plane misalignment.
The patient was prescribed a rigid, low-profile 3D designed custom orthosis to be worn each day on a part-time basis. The patient has been wearing the brace during the day for the past 10 months. Clinical and radiological findings from the most recent follow-up appointment indicate that the patient’s scoliosis has been stabilised and that the postural alignment has been improved. The patient reports that she now has less pain and has more mobility since wearing the brace.
Case Background
The 56-year-old female patient was referred to the ScoliCare clinic by her general practitioner. The patient had been diagnosed with scoliosis, on top of several pre-existing comorbid illnesses, 18 months prior. The patient reported that she had been experiencing significant pain for the past 10 years.
The patient lived on an isolated property and reported that she was having increasing difficulty walking around on the steep terrain. The pain that she was experiencing was also disrupting her sleep. The patient was no longer working due to back pain and could only perform limited house work because of her condition. Standing or walking for any length of time would also cause the patient to experience severe pain. Financial and geographic constraints prohibited the patient from being able to receive regular care or attend therapeutic exercise/rehabilitation classes.
Examination Findings
A detailed history and physical examination were performed. The pertinent findings from the history included a compression fracture at L3 two years prior which had prompted a bone mineral density assessment.
The patient had been classified as osteopenic based on findings from a DEXA scan. The patient had been diagnosed with chronic obstructive airway disease (COAD), asthma, Raynaud’s disease, scleroderma and systemic lupus erythematosus (SLE), temporal lobe epilepsy and varicose veins in the pelvis. Significant degenerative change in the mid-lumbar spine had caused the patient several bouts of radiculopathy and lower limb neuropathy for which she had received previous facet injections and radio-ablation therapy. The patient denied any family history of scoliosis and was not aware of the presence of any spinal deformity when she was younger.
The patient had been fitted with a pacemaker at age 31. The referral letter sent by the patient’s GP listed 21 different prescription medications. The patient stated that one or more of these medications was causing her to be chronically constipated for the past four years. The patient also reported that she was a smoker.
The physical examination revealed anterior sagittal balance and right coronal imbalance in the postural assessment. There was an increased waist curve on the right, decreased lumbar lordosis and evidence of spinal curvature in the lumbar spine (Figure 1).

Figure 1: Posteroanterior postural photograph (Left), Lateral postural photograph (Right).
Physical examination revealed a generalised decrease in the lumbar range of motion with left lumbar lateral flexion markedly reduced. The Adams forward bend test produced humping in the left paraspinal soft tissues. There was no evidence of pelvic, sacral, or lower limb deformity. The patient’s neurological exam was unremarkable.
The patient had brought several forms of diagnostic imaging to the initial consultation. Plain films taken 10 months prior portrayed a 38° (Cobb) left lumbar scoliosis (Apex L2). Laterolisthesis was noted at L3/4 and significant spondylosis from L2-L5 (Figure 2).
The most recent films indicated that the patient’s scoliosis had progressed, now measuring 51° (Cobb). Computed tomography confirmed the findings from the x-ray and highlighted vacuum phenomena at L2/3 and L4/5 intervertebral disc levels.
The patient was diagnosed with a de novo degenerative lumbar scoliosis.
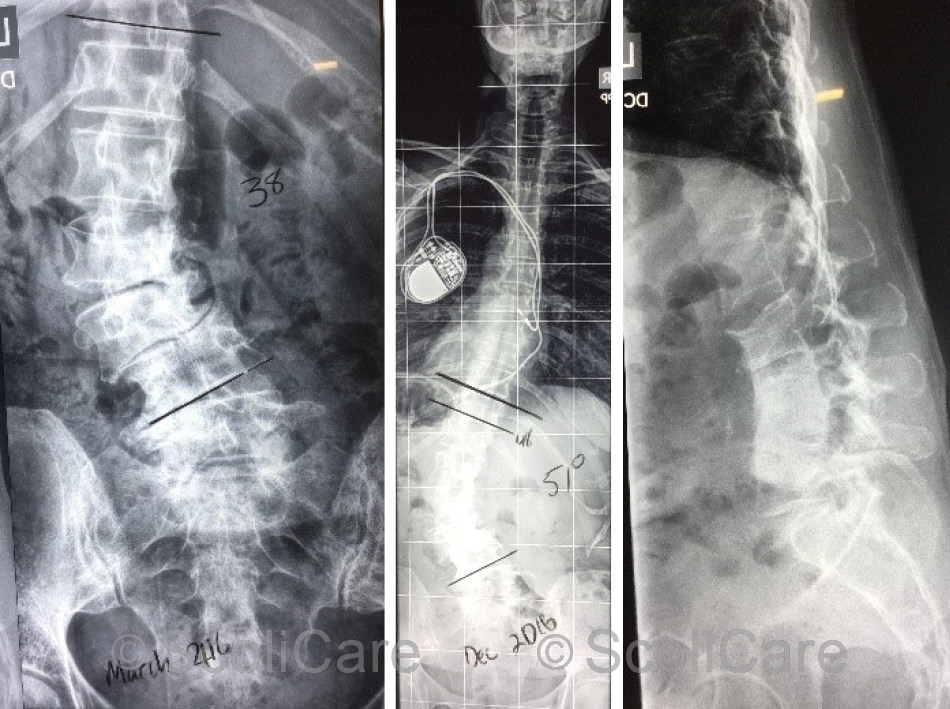
Figure 2: Posteroanterior spine x-ray highlighting a 38° (Cobb) left lumbar scoliosis taken 10 months prior to the initial consultation (Left), Recent posteroanterior full spine x-ray highlighting a 51° (Cobb) left lumbar scoliosis (Middle), Recent lateral lumbar x-ray (Right).
Intervention
The patient was prescribed a 3D customised, rigid, low-profile orthosis designed to correct/stabilise the deformity in the lower spine. The brace was fitted three months after the initial consultation.
In-brace photos taken at the time of the brace fitting demonstrated a significant improvement in the patient’s sagittal and coronal postural balance. In-brace x-rays taken soon after the brace fitting appointment indicated a reduction in the patient’s scoliosis and an improvement in the sagittal balance (Figure 3). The patient was provided with instructions for donning and doffing and cleaning the orthosis. Brace wear was gradually increased by two hours each day up to the patient’s tolerance.
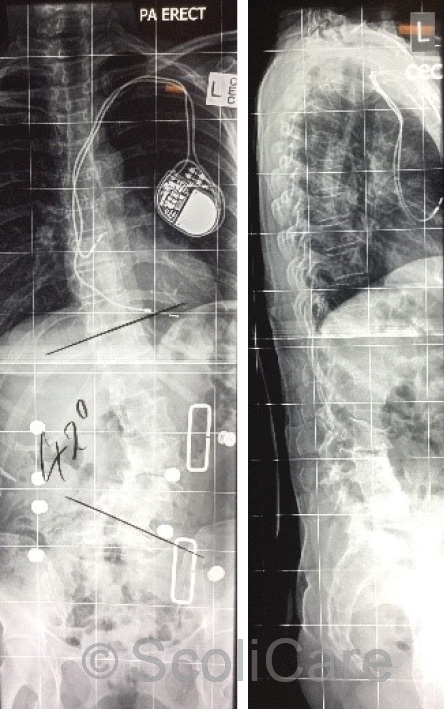
Figure 3: Posteroanterior in-brace x-ray with a 42° left lumbar scoliosis (Left),
Lateral in-brace x-ray highlighting an improvement sagittal balance (Right).
Outcomes
The patient attended a follow-up consultation one month after the brace fitting. The patient reported that overall the symptoms had been reduced by wearing the brace. The patient was reviewed again six months later. At this time, the patient stated that they were able to wear the brace for most of the day. The patient was still experiencing some pain but reported that their mobility was much improved in the orthosis.
The postural improvements displayed initially in-brace have been maintained (Figure 4) and the patient’s lumbar scoliosis has remained stable at 50° (Figure 5).
The patient is still under care and has been advised to continue with bracing during the day. To counteract the deconditioning that has occurred over the past decade, the patient has been instructed to begin performing some light exercise whilst wearing the brace.
The patient will be reviewed again in six months, but it is likely that she will be required to continue the current dosage of bracing indefinitely to preserve her current mobility. It is hoped that the brace will limit the progression of the degenerative changes that are associated with her scoliosis.

Figure 4: Posteroanterior postural photograph out-of-brace (Left),
Lateral postural photograph out-of-brace (Right)
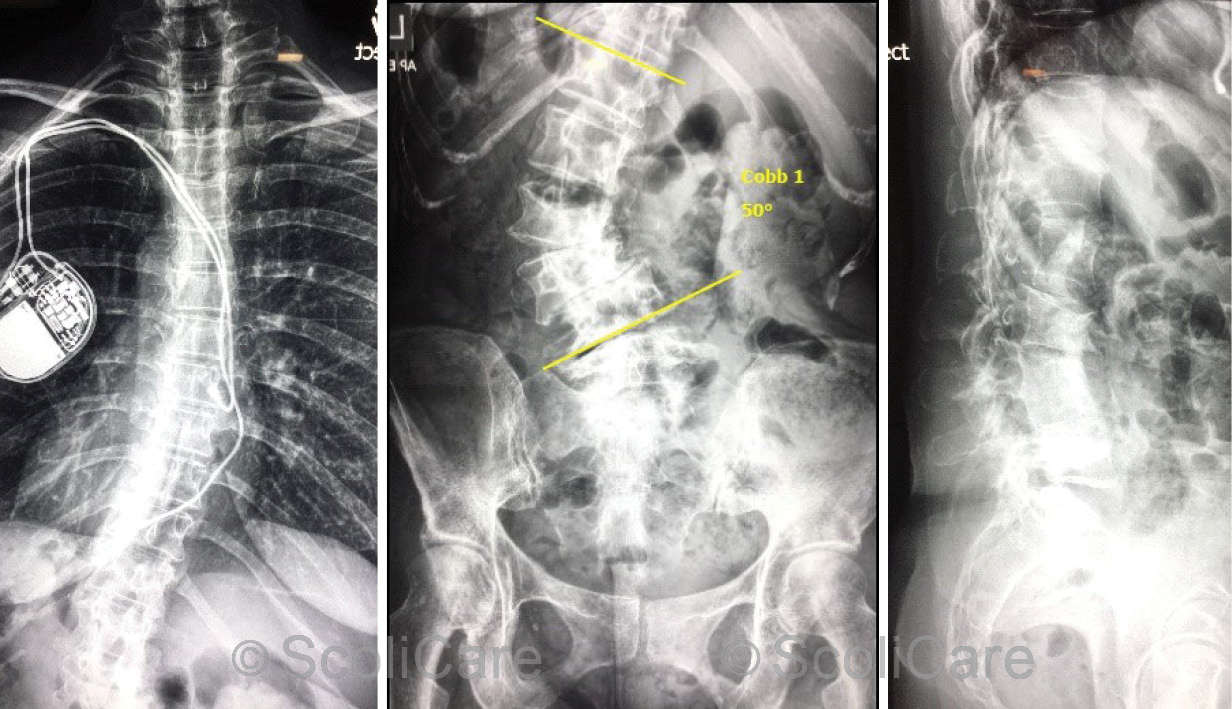
Figure 5: Posteroanterior thoracic spine x-ray out-of-brace (Left), posteroanterior lumbopelvic x-ray out-of-brace highlighting a 50° left lumbar scoliosis (Middle) Lateral lumbar
Discussion
The subject of this case study represents a typical de novo degenerative scoliosis presentation. The condition affects the thoracic and/or lumbar spine causing varying degrees of deformity, back pain, radicular leg pain and activity limitation.
The symptoms experienced by the patient in this case had led to a progressive decline in functional capacity, with the patient being unable to work, exercise, perform home duties, or ambulate around the grounds of her property. The radiological findings in patients with adult spinal deformity are particularly telling, with alterations in coronal and sagittal balance being commonplace. This abnormal placement of the body’s centre of gravity leads to excessive energy expenditure when the patient stands or moves and is often associated with disabling pain.
Shifts in spinal alignment accelerate the degenerative process leading to postural collapse and eventual compromise of the neurovascular structures around the spine. Decreasing bone mineral density and the presence of comorbid illness in this population further complicates the situation. In fact, the health status of many patients in this group is such that surgery is no longer a viable treatment option. Instead, conservative treatment strategies such as bracing are used to improve spinal alignment and maintain quality of life.
The treatment outcomes in this case are fairly representative of the outcomes in the adult spinal deformity population. Postural alignment, in particular sagittal balance, has been improved by the brace, which has translated into better mobility and reduced pain in this patient. The scoliosis which had been progressing at a rapid rate prior to initiating treatment has also been stabilised as a result of the bracing regimens.
Conclusion
This case demonstrates the successful management of a 56-year-old female patient with de novo degenerative scoliosis using a low profile 3D designed custom orthosis. The patient demonstrated good compliance with the brace and has experienced improvements in posture, mobility and pain.
NB: Results vary from case to case. Our commitment is to recommend the most appropriate treatment based on the patients type and severity of scoliosis.
© ScoliCare

